Transcranial Direct Current Stimulation (tDCS): Protocol Development and Clinical Applications
 Introduction
Introduction
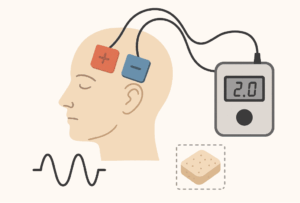
Transcranial direct current stimulation (tDCS) is a form of non-invasive brain stimulation that modulates cortical excitability using low-intensity electrical currents delivered through scalp electrodes. Since the pioneering work of Nitsche and Paulus (2000), who demonstrated polarity-dependent modulation of motor cortex excitability, tDCS has been studied extensively in psychiatry, neurology, and cognitive neuroscience.
The growing evidence base has spurred interest in standardized tDCS protocols, both for experimental reproducibility and for translation into clinical practice. The following review outlines scientific principles, protocol parameters, disorder-specific applications, safety standards, and emerging directions.
Neurophysiological Basis
-
Polarity-Dependent Effects:
-
Anodal tDCS reduces neuronal membrane potential, leading to subthreshold depolarization and increased likelihood of action potential generation.
-
Cathodal tDCS increases membrane potential, inducing relative hyperpolarization and decreasing cortical excitability.
-
-
Mechanisms Beyond Polarity:
-
Modulation of NMDA receptor activity.
-
Shifts in GABAergic and glutamatergic balance.
-
Influence on oscillatory network dynamics and long-term potentiation/depression (LTP/LTD)-like plasticity.
-
-
Dose-Response Relationship: Current density, electrode montage, stimulation duration, and repetition frequency interact to determine net outcomes.
General Protocol Parameters
| Parameter | Typical Range | Notes |
|---|---|---|
| Current intensity | 1–2 mA | Doses >2 mA not well established for safety in long-term trials. |
| Duration | 20–30 min | Prolonged stimulation >40 min risks homeostatic reversal effects. |
| Electrode size | 25–35 cm² | Smaller electrodes produce more focal stimulation but higher current density. |
| Session frequency | Daily / alternate-day | Cumulative effects seen after 5–10 sessions; protocols often run 2–4 weeks. |
| Current density | ≤0.08 mA/cm² | International safety guidelines threshold. |
Disorder-Specific Protocols
1. Major Depressive Disorder (MDD)
-
Montage:
-
Anode → left dorsolateral prefrontal cortex (F3, 10–20 EEG system).
-
Cathode → right supraorbital area (Fp2).
-
-
Parameters:
-
2 mA, 20–30 minutes, 10–20 sessions.
-
-
Evidence: RCTs (e.g., Brunoni et al., 2013; Blumberger et al., 2012) demonstrate moderate antidepressant efficacy, particularly as augmentation to SSRIs.
-
Mechanistic Rationale: Left DLPFC hypoactivity in MDD; anodal stimulation enhances prefrontal regulation of limbic circuits.
2. Schizophrenia – Auditory Verbal Hallucinations
-
Montage:
-
Cathode → left temporoparietal junction (T3).
-
Anode → contralateral supraorbital area.
-
-
Parameters:
-
2 mA, 20 minutes, typically accelerated twice-daily sessions for 5–10 days.
-
-
Evidence: Systematic reviews indicate modest efficacy in treatment-resistant hallucinations, though inter-individual variability remains high.
3. Neuropathic and Chronic Pain
-
Montage:
-
Anode → primary motor cortex contralateral to pain (C3 or C4).
-
Cathode → supraorbital region.
-
-
Parameters:
-
1.5–2 mA, 20 minutes, 5–10 daily sessions.
-
-
Mechanistic Rationale: M1 stimulation modulates thalamo-cortical circuits and descending inhibitory pain pathways.
4. Cognitive Enhancement (Stroke, MCI, ADHD)
-
Montage:
-
Anode → left DLPFC (F3).
-
Cathode → right supraorbital area.
-
-
Parameters:
-
1–2 mA, 20 minutes, 5 sessions/week for 2–4 weeks.
-
-
Evidence: Moderate improvements in working memory, attention, and executive function, particularly when paired with cognitive training tasks.
Safety and Tolerability
-
Adverse Events: Most common are mild scalp tingling, itching, erythema, and transient headache. Serious adverse events are rare.
-
Safety Thresholds:
-
Current ≤2 mA.
-
Session duration ≤40 min.
-
Current density ≤0.08 mA/cm².
-
-
Contraindications: Implanted neurostimulators, pacemakers, epilepsy (relative), open scalp wounds, pregnancy (precautionary).
-
Long-Term Data: No structural brain damage demonstrated in MRI/EEG follow-ups extending up to 1 year.
Emerging Directions
-
High-Definition tDCS (HD-tDCS): Use of smaller electrodes in ring configurations for focal stimulation.
-
State-Dependent Stimulation: Adjusting protocols based on ongoing EEG/fNIRS activity.
-
Home-Based tDCS: Feasibility trials for depression and cognitive decline; raises concerns of adherence and misuse.
-
Personalized Medicine: Incorporating computational modeling and MRI-based electric field mapping to optimize electrode placement.
-
Combination Therapies: Synergistic effects when combined with rTMS, cognitive remediation, or pharmacotherapy.
Conclusion
tDCS offers a scientifically grounded, low-cost, and safe neuromodulatory technique with applications across psychiatric and neurological disorders. While protocol standardization has improved, individual variability in responsiveness underscores the need for personalized stimulation strategies and integration with behavioral interventions. Continued refinement of protocols, supported by neuroimaging and computational models, is likely to enhance both efficacy and precision in the coming years.
✦ About the Author
I’m Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi), Consultant Psychiatrist in Chennai. At our clinic, we focus on a holistic approach to mental health, combining pharmacotherapy, psychotherapy, ketamine therapy, and other evidence-based interventions. My expertise includes neuromodulation techniques such as rTMS, tDCS, and neurofeedback, which I integrate into clinical practice alongside standard psychiatric care. These are complemented by insights from nutrition, lifestyle, and allergy management to provide comprehensive, individualized treatment.
📍 Mind and Memory Clinic, Apollo Clinic, Velachery, Chennai (Opp. Phoenix Mall)
📞 +91 85951 55808
🌐 srinivasaiims.com