Sertraline for OCD During Breastfeeding: What Parents Need to Know
Becoming a parent brings joy, responsibility, and profound change. For some, it also brings a worsening or new onset of Obsessive-Compulsive Disorder (OCD)—especially in the perinatal period. When intrusive thoughts and compulsive behaviours begin to interfere with bonding, sleep, and daily functioning, treatment becomes not only appropriate, but essential.
One of the most common concerns parents raise is:
“Can I take medication and still breastfeed safely?”
Sertraline is often the answer. Here’s why.
What is sertraline, and why is it used for OCD?
Sertraline is a selective serotonin reuptake inhibitor (SSRI). SSRIs increase the availability of serotonin in key brain circuits involved in mood regulation, threat detection, and habit formation.
In OCD, these circuits become overactive and rigid. Sertraline helps reduce:
-
Intrusive, repetitive thoughts
-
Anxiety driven by uncertainty or fear
-
Compulsive behaviours used to neutralise distress
It is one of the most evidence-based medications for OCD, across age groups and clinical settings.
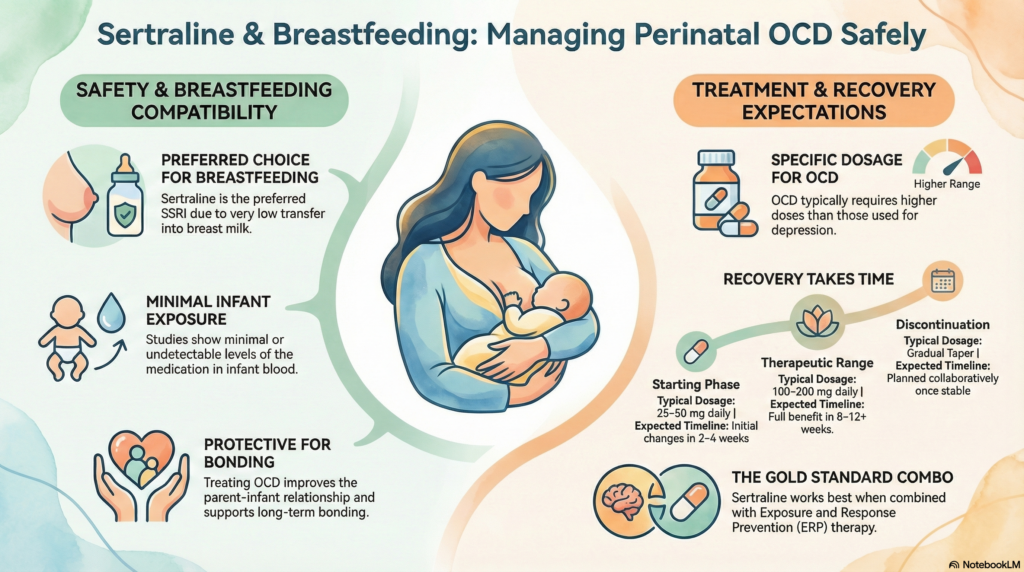
Is sertraline safe during breastfeeding?
Yes. Sertraline is widely regarded as the preferred SSRI for breastfeeding parents.
What makes it reassuring:
-
Very low transfer into breast milk
-
Minimal or undetectable levels in infant blood
-
Decades of real-world use with a strong safety record
Because of this profile, sertraline is often recommended first by perinatal psychiatrists and specialist guidelines.
Will sertraline affect my baby?
In the vast majority of cases, no significant effects are seen.
Occasionally, some infants may show:
-
Mild sleepiness or fussiness
-
Transient feeding changes
These effects, when they occur, are usually short-lived and mild. Serious adverse outcomes are rare. Monitoring is typically simple and precautionary rather than intensive.
Do I need to stop breastfeeding if I take sertraline?
No. In most situations, breastfeeding can safely continue.
This is an important point:
Untreated OCD can interfere with bonding, increase distress, and prolong suffering. Treating the parent’s mental health often improves the parent–infant relationship, which is a protective factor for both.
Can sertraline be started for the first time while breastfeeding?
Yes. Sertraline can be initiated postpartum, even if you have never taken it before.
It is commonly prescribed for:
-
Postpartum OCD
-
Postnatal depression
-
Postpartum anxiety disorders
Starting treatment under medical supervision allows careful dose titration and symptom monitoring.
What dose is usually needed for OCD?
OCD typically requires higher doses than depression.
-
Starting dose: 25–50 mg daily
-
Effective OCD dose range: 100–200 mg daily
-
Dose increases are done gradually, based on response and tolerability
Slow titration helps reduce side effects and improves adherence.
How long does sertraline take to work in OCD?
OCD improves more slowly than depression.
-
Early changes may appear in 2–4 weeks
-
Meaningful improvement often takes 8–12 weeks
-
Full benefit may take longer, especially in longstanding OCD
This delay does not mean the medication is failing—it reflects how OCD circuits adapt over time.
Is therapy still necessary?
Yes. Medication works best when combined with Cognitive Behavioural Therapy (CBT), specifically Exposure and Response Prevention (ERP).
ERP helps retrain the brain to tolerate uncertainty and reduce compulsive responses. The combination of sertraline + ERP offers the strongest and most durable outcomes.
What if I want to stop sertraline later?
Sertraline should never be stopped abruptly.
When symptoms are stable and the time is right:
-
The dose is tapered slowly
-
This reduces withdrawal symptoms
-
It also lowers the risk of relapse
Discontinuation is a collaborative, planned process—not a sudden decision.
A final word
Perinatal OCD is common, treatable, and nothing to be ashamed of. Needing medication during breastfeeding does not mean you’ve failed—it means you are taking care of your health so you can care for your child.
Sertraline, when appropriately prescribed and monitored, allows many parents to recover without sacrificing breastfeeding or bonding.
About the author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
Dr. Srinivas specialises in perinatal mental health, OCD, anxiety disorders, and evidence-based psychotherapy. His clinical approach integrates medication, CBT-ERP, psychoeducation, and digital tools to support recovery while respecting individual values and family contexts.
✉ srinivasaiims@gmail.com
📞 +91-8595155808